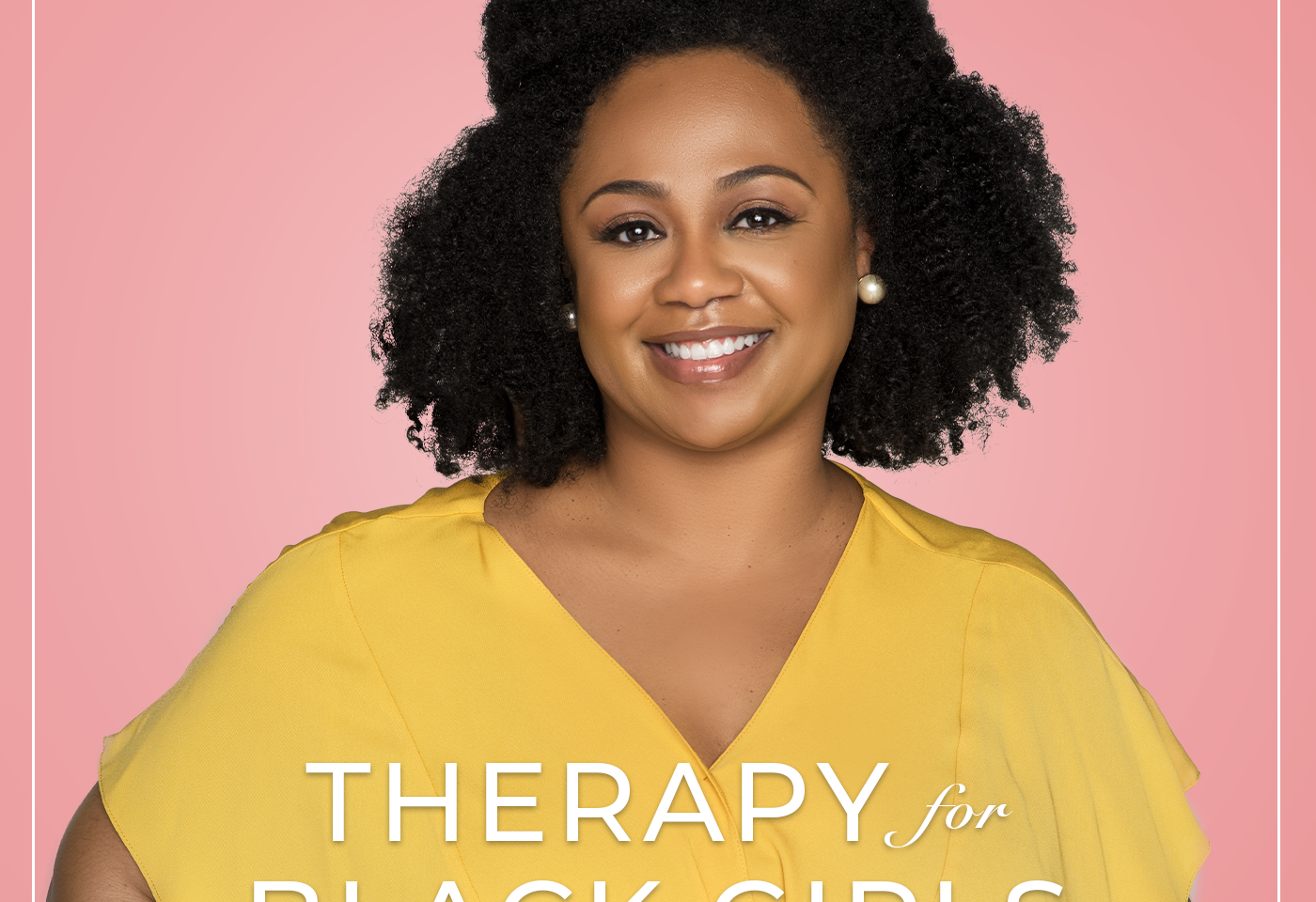
The Therapy for Black Girls Podcast is a weekly conversation with Dr. Joy Harden Bradford, a licensed Psychologist in Atlanta, Georgia, about all things mental health, personal development, and all the small decisions we can make to become the best possible versions of ourselves.
Last month, psychiatrist Dr. Karinn Glover, joined us in the Sister Circle for a conversation all about psychiatric medications and shared such valuable information that I wanted to share it with as many of you as possible. Our community manager, Jasmine Jones, joined her for this conversation and they chatted about when you might consider talking with a prescriber about medications, some common side effects of psychiatric medications, what kinds of information you should share with your prescriber to get the best medication for you, and general timelines for how long someone might take medication. It’s important to note that all of the information Dr. Glover shared was generally speaking. You should talk to your healthcare providers about any specific concerns.
Resources
Visit our Amazon Store for all the books mentioned on the podcast!
Join us for the Last Days of Summer Book Club chat on Aug. 26 @ 7pm EST. therapyforblackgirls.com/bookclub.
Where to Find Dr. Glover
Twitter: @drkarinn
Instagram: @drkarinn
Stay Connected
Is there a topic you’d like covered on the podcast? Submit it at therapyforblackgirls.com/mailbox.
If you’re looking for a therapist in your area, check out the directory at https://www.therapyforblackgirls.com/directory.
Take the info from the podcast to the next level by joining us in the Therapy for Black Girls Sister Circle community.therapyforblackgirls.com
Grab your copy of our guided affirmation and other TBG Merch at therapyforblackgirls.com/shop.
The hashtag for the podcast is #TBGinSession.
Make sure to follow us on social media:
Twitter: @therapy4bgirls
Instagram: @therapyforblackgirls
Facebook: @therapyforblackgirls
Our Production Team
Executive Producers: Dennison Bradford & Maya Cole
Producer: Cindy Okereke
Assistant Producer: Ellice Ellis
Session 221: A Conversation About Psychiatric Medications
Dr. Joy: Hey, y'all! Thanks so much for joining me for session 221 of the Therapy for Black Girls podcast. We'll get right into the episode after a word from our sponsors.
[SPONSORS’ MESSAGES]
Dr. Joy: Last month, psychiatrist Dr. Karinn Glover joined us in our Sister Circle community for a conversation all about psychiatric medications and she shared such valuable information that I wanted to share it with as many of you as possible. Dr. Glover graduated from Howard University with a BA in History and then worked at Essence Magazine and as an account executive for Verizon. She followed her curiosity about medicine and ultimately attended SUNY Downstate College of Medicine and obtained a Master of Public Health from Columbia University's Mailman School of Public Health, via the highly competitive Macy Scholars Program. She's currently an Assistant Professor of Psychiatry at the Albert Einstein College of Medicine and teaches psychopharmacology and aspects of psychotherapy to Psychiatry and Family Medicine residents.
She's also an attending psychiatrist in the adult outpatient psychiatry department at Montefiore Health System. She uses mindfulness-based techniques in her psychiatry practice, in her career coaching for professionals from marginalized cultures, and her leadership of discussions of the impact of racism on physical and mental health.
The conversation you'll hear was between Dr. Glover and our community manager, Jasmine Jones. They chatted about when you might consider talking with a prescriber about medications, some common side effects of psychiatric medications, what kinds of information you should share with your prescriber to get the best medication for you, and general timelines for how long someone might take medication.
It's important to know that all of the information Dr. Glover shared was generally speaking and that, for your specific concerns, you should talk to your healthcare providers. If there's something that resonates with you or something you think others should know while enjoying the conversation, please don't forget to share it on social media using the hashtag #TBGinSession. Here's the conversation.
Jasmine: I'm so excited to get into this conversation with you, Dr. Karinn. I think it's a much-needed conversation. I guess we can jump right into what doctor *[inaudible 0:04:53] was saying about hesitation and just the history of non-ethical medical practice in the United States, something that is very real and can cause anxiety for maybe someone who actually would benefit from medication. Can you just speak to how you would help someone to come to terms with being okay with having medication and just some comforting facts about the research and work that you're personally doing that would benefit black women?
Dr. Glover: Yeah, thank you. A lot of stuff comes out in my first and second assessments with a patient. The first time I see somebody, it's usually an hour or an hour and a half and from there, we're talking about how they've been doing and the impact of their depression or their anxiety on their life right now. When we get down to like how this is affecting them and the consequences if it goes untreated, that's kind of where medication comes into the picture. First of all, I love to make sure that all my patients have access to psychotherapy if they want to and if they're motivated. And then if somebody is not interested in psychotherapy, then I'm like, okay, can we think about other ways to take a holistic approach to this?
Then some people will say I'm open to everything, so then I'll say, all right, are you interested in exercise? Are you interested in other self-care practices that have been shown to improve your mood? So can we make sure you get sunlight? Can we make sure you get outside in nature and do some forest bathing, just getting around some trees? Can I make sure that you get to hang around loved ones who affirm who you are?
And so once we make sure that we're taking a holistic approach, and we think through their diet and their exercise regimen and whether they've got a good diet and lots of green vegetables and mushrooms and things like that, sardines, all the nutrients. After we make sure you’ve got all the nutrients, all the family love, then the question comes–all right, would you consider medication? Because sometimes the stakes are really high so there are some people who are at risk of losing their job because their depression is so bad that they can't focus. They are at risk of losing their job because their social anxiety is so intense, they won't go on public transportation. Or they won't show up for work because perhaps work requires that you talk and interact with the public.
So if I know that you're about to lose your job, if I know your depression is so bad, you're not responsive to your growing babies, then we need to think about taking more, I think, stronger action and so that's where medication also comes in. I openly acknowledge that medicine, including psychiatry, has not always been kind to black people. I know that experiments were done, that surgeries were forced on us, that there's been coercive tactics to get people to take medication and to participate in medication trials that we did not give consent to. And so I start by acknowledging that for the patient because often, I think growing up, we hear about those stories and yet how do we reconcile the history of medicine with who's standing in front of me telling me, maybe you want to try this Lexapro or this other medication?
I try to just put it all out there for the patient and make sure that she knows that she can ask me about that and whatever I don't know, we can talk through and I'll look up or I'll research, I'll talk to experts. And so from there, we just tried to figure out like what are the consequences? What's the impact? What are our goals? And then what's going to work? And sort of like what are the conditions we're working under? And so I'm sure we're gonna get to more of that but that's sort of where I start.
Jasmine: Absolutely, thank you so much for acknowledging that. Let's talk about the different classes of drugs that you will be prescribing (as) psychiatric medication.
Dr. Glover: For sure. I prescribe them all, really. Meaning there's medications that we use... Let’s just say in medicine, we often find that medications are effective in advertent ways, sometimes even by accident. Something like lithium, we found out that lithium was good for bipolar disorder because we were trying to use it for something else. And then we found out it made the bipolar folks calmer and better able to function. So in the history of medications, we often find that they can be used for two things. There are some antibiotics that are oddly good for depression. There are antipsychotics that are helpful for psychosis but also for bipolar disorder, and also to help with depression.
Bear in mind that even though there are classes of psychotropic medications, we sometimes do a little bit of cross pollination. We may use something that has indications for three different things, we may use it for something else, so let's bear that in mind. So I prescribe medications for psychosis and psychotic disorders like schizophrenia. For schizoaffective disorder, I prescribe medications for anxiety, so that includes medications like Xanax, which often you hear rappers talk about or housewives (the housewives of lots of different places talk about it openly on television!) I prescribe medications that can be used for seizure disorder but also for bipolar disorder. And of course, antidepressants.
Jasmine: Perfect. And then are there some drugs that are less effective for black women but still being prescribed?
Dr. Glover: I'm gonna say no-ish. Because I think the field of pharmacogenetics is sort of still growing. Typically, the studies that were done to assess pharmacogenetics were based on the researchers’ assumptions about who's black and who's not. And as you well know, just because you look black doesn't mean that is the only thing that is genetically making up who you are. Some of what we call alleles that govern how a receptor bends or responds in the presence of a drug, sometimes those may come from a white ancestor or an Asian ancestor and not the African ancestor. But you still may have kinky, coily hair, full lips, and look black and present as black. And so I have come to not really rely on pharmacogenetics or phenotype to figure out what works for the patient.
There are some rather expensive studies that can be run to figure out which antidepressants or which medications might be more effective but that field is so new and so expensive, and I work in the South Bronx where that's just not feasible. For me, the best way to figure out if a medication is working is to check in with my patient and say, are you able to get out of bed? Did you get dressed? Were you able to accomplish the things you wanted to accomplish yet? Unfortunately, sometimes my ability to predict, or wish for the medication to work, does not happen within six or eight weeks and then we have to try something else. And I recognize that that can be very, very difficult.
Jasmine: When I hear you say six to eight weeks, you're saying that is typically the amount of time where you would then switch. So you give it that much time to feel a difference? We’re not expecting “okay, we’re two weeks in now, I should feel better.”
Dr. Glover: Yeah, it depends on the medication. There are some medications that work sooner. If somebody is presenting to me with intense anxiety and we try something, there's a subset of people, usually 20% of people, who try a medication like an SSRI or an SNRI who may feel an effect within five or so days. And then there's the rest of us who may not feel anything for a week or two or three. If a person doesn't feel anything by four weeks–even if we increase it, even if they're tolerating the side effects–then I start to go like, hmm, I'm not sure.
I may try to optimize the dose, meaning get the dose towards the maximum, assuming they're not having side effects or that the side effects are not intolerable. So assuming they can tolerate whatever is happening, maybe a little bit of sedation or other side effects we can talk about. But if I know that they can tolerate it, then I'm going to try to work with one medication and try to get it as high as possible to treat the symptoms. And that's also where psychotherapy comes in because I think everybody on here knows that psychotherapy can be quite impactful for people who are motivated and willing to show up for it. And it does what antidepressants also do, it sometimes just takes longer to see an effect. But sometimes the combination of the two can be much more effective and efficient than doing one or the other.
Jasmine: So a person who is interested in getting medication, they don't necessarily have to like go through a whole process of speaking with a therapist first or having multiple visits with their psychiatrist. How would you go about diagnosing someone? And then about how long from you diagnosing them until them being actually on the medication, does that typically look like?
Dr. Glover: It depends on the setting. There's a model of care called collaborative care that we do at Montefiore where people go... First of all, the wait to see a psychiatrist is really long. The wait to see any kind of prescriber is often months long. At the clinic where I work, it's unfortunately like four months to get in to see a psychiatrist. So in that case, sometimes people go to their primary care doctor because we know that primary care doctors do the overwhelming bulk of the prescribing of psychotropic medications in the United States. It's not psychiatrists. There's only like 820 black psychiatrists and there's like 11,000 psychiatrists in the United States so we know that lots of work is done by a primary care doctor.
Some people go to their primary care doctor, they go and get their blood pressure checked, they go to get their Coumadin checked or whatever. They got to their OB or their GYN doctor and say like maybe they get assessed as part of like triage and it may come out that they have some depressive symptoms. Sometimes the work gets done there, especially if there's a social worker there who may commence or start off doing psychotherapy or that kind of assessment. And then that social worker may say, “Hey, this person's not benefiting from seeing me. It's been four or six weeks, maybe they need to see a psychiatrist,” and then they'll get referred. So there's that style which is collaborative care.
And sometimes that OB or that GYN or that internist or that family medicine doc will call me and say, hey, Karinn, I have this patient, look at their chart, the social worker’s written this beautiful assessment. I'll look at the assessment and I'll say, oh, clearly, this is a 28-year-old woman who wants to get pregnant, she's in a relationship and she is perhaps struggling with appetite. And so she's lost a lot of weight, okay, I can think of one medication that could be really helpful for her, and I'll tell the OB or I'll tell like other clinician, try this medication. And so I will have never seen the patient, but guess what, that patient is getting the medication from a prescriber and they're being monitored by a therapist in primary care. That's one way to get people access to the medications.
Then there's seeing me, which again, sometimes takes a terribly long amount of time. And as a black woman psychiatrist, we're like unicorns, there's so few of us. When somebody finally gets to see me, that usually means their symptoms are pretty severe and so, in that case, have they tried other medications? Do I have to like find some new combination? Seeing them for the first time, it depends on how urgent it is, I may start them on something the day that I see them and ask them to go pick up a prescription. And then after that, I'll try to see them weekly or every two weeks at least to touch base or through telemedicine, to find out how they're doing, what their symptoms are like. And then sometimes they're feeling better within three weeks or, you know, by the end of the month we're seeing small changes.
Dr. Joy: More from our conversation with Dr. Glover after the break.
[BREAK]
Jasmine: One of the questions that you had sent me over that you hear a lot and I just thought of while you were talking about that with the trial and error process, is people saying that how do I know I'm not just being experimented on? Can you kind of talk (about) like the process of companies doing their own trials? And how if you could ever end up in that situation and not know it.
Dr. Glover: That should never happen. Any time there is a study going on, there's a whole consent process that has to be created and approved by the institutional review board of whatever institution is doing the study. At any point, if anybody is in the study, they know they are in a study. They may not know whether they're receiving a placebo or not but that has been discussed ahead of time. There is no way you're swallowing a pill that has been given to you by me, and finding out later that it was nothing or that this is an experiment of some evil scientist.
The way, unfortunately, that psychiatry gets depicted in popular films and television is often that we are corrupt, that we are secretly trying to have sex with our patients and all kinds of like terrible stereotypes. So it's a lot to show up every day and just be like, none of that is real, I'm actually a decent person and I really just want to make you feel better. However, there are times when I cannot predict which medication will work and I can say, look, I can think of medications that can be helpful that are likely to help you. If you can tolerate any potential side effects that come up, I will work with you to find something that will help you have the life that you want to lead. If the medication is not helping you and you don't want to take it, please let me know and we will find something else. I take no pleasure in other people's suffering. And I think other psychiatrists are similarly minded. Like nobody's out here trying to cause suffering.
Jasmine: I love to hear that. If you've been taking medications for several years, will it at some point be necessary to have an adjustment in the dosage or even just changing medications in general?
Dr. Glover: Sometimes, it is necessary to change medication or to change the dose. It depends on pregnancy status, it depends on other comorbid conditions. Like if you develop high blood pressure and we know that there are some medications that at very high doses, the high end of the dose range can be linked to hypertension. We’ll monitor you differently than if you were perhaps on a lower dose or if you were in a different age range. I'd say the simplest answer is like it depends.
And it also depends on lifestyle changes. If you know that you were previously on a medication that made you sleepy but you need to pick up nighttime work for whatever reason. You're a nurse and you suddenly go from working days to nights, then would I want you to be on that medication knowing that you're driving home perhaps impaired by sleep deprivation and about to take this medication that might make you a little bit sedated? And you've got to also be there for your kids if you're a single parent, things like that I take into account, so that's one thing.
And then I have had some patients who were on one medication for quite a long time and then they felt like, out of nowhere, it stopped working. I'm reluctant to change medications but sometimes I'll change to like a sister or a cousin medication. Or I may think of adding something else from a different class to sort of boost the effect of the original medication.
Jasmine: How do you have conversations with your partner, your family, even your children sometimes, about the potential side effects of a new medication that you're trying? Some of the things here are weight gain and sexual dysfunction.
Dr. Glover: I often try to normalize for my patients that if you have high blood pressure, there are certain high blood pressure medications that make you sensitive to sunlight, so you know you have to wear sunscreen or you know you can't lay out in the sun with your kids. Medications for mental health are similar in that way. They're related to biochemical changes in the body and the brain, just like high blood pressure medications, just like statins we use to lower cholesterol.
I find that when people understand that mental health issues are a mind-body issue, not just a mind or a spiritual issue, then it helps people find their grounding to have conversations with other people. I say the first thing I say to people is... And I ask them like, does your family know that you're on medication? And they'll say, “you know, I feel kind of funny telling them.” And then I’ll ask, what makes you feel funny? Okay, your family may see this as a spiritual failure that you are on medication. Your family may see this as a weakness. But would they say that to you if you fell and broke your ankle? Would they say if you only prayed harder, your ankle would heal quicker or you wouldn't feel any pain at all? Hmm, right?
So we kind of have to talk through some of the biases that we grew up with and then we have to talk through how do you shape that conversation to honor your experience as somebody who is dealing with a mind-body issue? And how do you simultaneously let them know after I take my medication, by 9pm, I need to be asleep. If I have bipolar disorder, I have to sleep so I need help with the kids because if I don't get my sleep, I might be at risk for a manic episode and those can be disastrous. If I don't get the right amount of sleep or if I don't get the right nutrition while I deal with my depression, that could set me back and that's only going to make me feel worse. So how can we make sure that we plan for the things that I need? To me, that's where you focus the discussion. It doesn't have to be about personal weaknesses and failures because that's not going to leave anybody feeling better.
Jasmine: If someone is dealing with a low sex drive because of a medication that they're taking, are you suggesting that they take something else to help with that or what is something that you recommend?
Dr. Glover: With SSRIs, the class of antidepressants that we often use for depression, there can be the potential for sexual side effects. And for women particularly... Women and men, but for women it can be hard. Because if we're in a heterosexual relationship where the man is particularly focused on helping his partner achieve orgasm and he is not comfortable using a toy to help his partner get there, it can leave the man feeling very defeated and leave the woman feeling like orgasmless or, as we say, anorgasmic. In that case, I do tell my patients ahead of time, like this medication might help you with your depression but if sex is the only thing you enjoy right now and you're terribly depressed, maybe we need to think about another medication. And I've had that conversation, y'all, with women in their 70s and 80s, okay?
I have a 70-something year old patient. We had to have her like take a little break from her SSRI for a weekend because she was like, I haven't had an orgasm in a decade. And she was like, look, we're just getting to know each other but you should know I want an orgasm. And I was like, girl, we’re gonna get you your orgasm. And yes, ma'am. She got her orgasm back and then some. So, yeah, we try to talk about those.
Jasmine: What you just said about stopping for a weekend, how do people typically stop medications? Like let's say your insurance changes or you don't want to be on any, whatever the reason is. You become pregnant. How do you go about stopping the medication that you've been taking for a long amount of time?
Dr. Glover: There are some medications... Particularly there's like one medication where you just don't miss a dose. And so I'm just being very honest with you, it's called Venlafaxine, it's also called Effexor. And it's really a lovely medication, works very, very well. Unfortunately, you miss a dose and suddenly you feel like you have the flu and a headache and a migraine, and all kinds of things. So you just don't miss a dose. If you want a decrease, we do it very, very slowly. And there are times where even we decrease and we get to a point where when we stop it, the person still has side effects or what we call discontinuation effects. And so sometimes we will switch to something that lasts much longer in the bloodstream, just to tide them over until we get down to zero–if they want to come off all antidepressants, particularly that one. We, again, do it slowly and if we need to, we switch to something else.
Jasmine: Is it normal for someone to be on a medication for 20–30 years or is an anti-depressant or something for anxiety something that you typically will be on for a while, work with a therapist, and then at some point get off.
Dr. Glover: It depends on the severity of the depression and how many episodes of depression the person has had. Because there's really good data to show that one episode of depression means, like the first thing I'm gonna say is go for psychotherapy. If you need medication, I'm here. If you're on medication and psychotherapy and you experience a remission of symptoms, then I will say I at least want to give this six months to work and to just see how life is with medication.
And because untreated depression, every episode of untreated depression, leaves a person more vulnerable to harder-to-treat depression in the future and at risk for cognitive impairment–in tiny ways, but... I think I can't underscore this enough that depression is a mind-body issue and so I try to make sure that people understand that every episode of depression needs to be treated. Either with psychotherapy or with medication or the combination of both, just don't leave it untreated. For most people, any episode of depression will probably end after one year but if it doesn't, it really, really needs to be treated.
And so if somebody has had more than two episodes of depression, if we say the first episode of depression happened, you stayed on your medication for six months, you stayed in therapy for six months, okay, fine. If you really want to drop us all and go live life, that's fine. You come back to me with a second episode of depression, I want you to stay on medication for a year and be in therapy, if you're willing. If you stop it after a year and then come back to me with a third episode of depression, I will recommend that you stay on medication for the rest of your life. Because every episode of untreated depression leaves a person at higher risk for depression in the future that may be harder to treat and they may have residual symptoms of some cognitive impairment.
Jasmine: Someone is in the process of trying to get pregnant: Do you adjust their dosage? Do you guys talk about what that looks like once they're pregnant? And does any medication that you're prescribing have effects on fertility and unborn babies?
Dr. Glover: When it comes to pregnancy and fertility, I'll start off with fertility. No, I believe that in each of the medications that we prescribe for any mental health disorder, I do not believe any of them can impair fertility. There's some anti-psychotics that may affect periods, but it's super-duper, extremely, extremely rare. And so for that matter, like we just try to think, okay, this person is of childbearing age and they are perhaps likely to be pregnant because they're not on a contraceptive. So then we'll just think, okay, if this person does get pregnant, we will immediately stop certain medications.
There's one antidepressant particularly, Paxil (paroxetine), that we try to make sure that people are not on when they're pregnant. There are also medications for seizure disorders and for bipolar disorder that have been shown to be what we call teratogenic, that can affect the spine of the baby and perhaps be related to some growth abnormalities as well. So we keep those things in mind for sure. But overall, SSRIs, antidepressants like from the SSRI class, have been shown to be fine, particularly when we're weighing the risk of depression or depressive illness with the risk to the baby. So the risk to the mother's health sometimes versus the risk to the baby.
Usually, we'll just say this mom needs to stay in therapy and on medication because they may have a history of suicidality, they may have a history of psychosis. And I am not here to say that folks who have dealt with mental disorders should not have children. Do you know what I'm saying? I'm out here like, look, you want to have this baby, we’re going to have this baby. This is gonna be the people's baby and we're going to do this. But I need to make sure that you're not going to hurt yourself and that the most important thing is that, when your baby is born, you are present enough to take care of this baby.
Dr. Joy: More from our conversation with Dr. Glover after the break.
[BREAK]
Jasmine: I would love to know who would you say is a good candidate for getting psychotropic medications and then who is maybe not so good of a candidate?
Dr. Glover: A few things. It depends on what the underlying disorder is. If we're talking about depression, if the person is not motivated for therapy, then I'm going to think, okay, how severe is the depression? If I can just say like exercise and take long baths and pray and read inspirational books, then I'll say that. But often, by the time people get to me, it's because they've tried all of those things and it hasn't been quite enough.
So from there, if they are motivated to take a medication or even if they are not so motivated but they're willing to at least try taking medication, three, four times a week... Because I'm not there, I'm not going to be feeding it to the person every morning. I know we as humans, I don't even take my vitamins every day, right? So if they are willing to try, I'm willing to meet them there. And so that person is a fine candidate to take and to try medications. Will I give them the thing that if they miss a day, they have horrible headaches and feel like they're coming down with COVID? No. I'm going to give them a medication that probably will last in their system for three, four or five days. For example, Prozac or fluoxetine, it stays in the system for days so if you miss a day, you won't feel any different. That's one thing I’d take into account–how likely is the person to remain adherent to the medication?
Jasmine: Thank you. Do you have any advice for someone who's like struggling to accept that they need to be on a medication for a long time?
Dr. Glover: I think often it's a conversation. It starts with, what's the hardest thing about accepting this? And then sometimes it has to go back to what were you taught about depression growing up? Or what were you taught about mental health growing up? And if you were taught that it's a sign of weakness or that it's a sign that it's only for people who need to be in institutions, that there's no spectrum of disorders, there's no spectrum of symptom severity, that there's only either you’ve got to pop an Instagram page or you are locked up in the inpatient unit, then we need to talk about, you know, sort of like getting away from black and white thinking. And we need to think about that there's a whole set of ways to live with a mental health disorder.
And then from there, it's really not something you have to accept for your whole life. You just have to accept it every morning when you take your medication or every night before you go to bed. There's plenty of things that people wish they could change about their bodies and their health and yet that's where, to me, mindfulness comes in as well, as an extra way to just learn how to not judge and to remain committed to yourself.
Jasmine: I'm not even sure if you could respond to this, but if you're able to. If you have a family member who had a bad experience with medication and you feel like they would benefit from being on it, how would you encourage them to do that?
Dr. Glover: I would wonder what happened. Meaning, was it the relationship they had with the prescriber? Was it the side effects that they had? Because often, I'll prescribe a medication and the patient doesn't really like it. The thing is, I try to set it up where people know that they can come back and tell me, hey, Dr. Glover, I didn't like this medication, you’ve got to give me something else. And people do that all the time. Because I can't promise that if I offer you like grilled cheese that you're gonna like it, you can say like I didn’t really like that, can I get something else? It's fine. So I do wonder whether that person's prescriber was open enough.
Assuming the prescriber was open and said please come back and tell me if this medication doesn't agree with you and I will work with you to manage the side effects. For some people, they try a medication that I think will not make them sedated so I will say it's probably better to take it during the day. Well, do I know every human on Earth and how a medication is going to affect them? No. So some people say, hey, I took your medication during the morning and I slept the whole day. Well, guess what? We're going to take it at night this time, right? Please, tomorrow, try taking it at night. And take it at 6pm so that by the time you wake up, the sedative effects have worn off and you're not groggy. I really do try to have that conversation with people and just say, just because you took it for a couple of nights and it made you feel weird, that doesn't mean we have to throw it away; it just means we need to adjust when and how you take it.
There's an antidepressant that we also use to prevent migraines, it's called amitriptyline. I have chronic migraines, I took amitriptyline, 10 tiny little milligrams. I woke up the next morning, I had slept for 13 hours, and I sat on the edge of my bed and I was like where am I? And my vision was blurry and I was like, these are all the side effects I learned about in medical school and they're all happening to me right now. And then I learned, okay, I need to, A, try this medication on a weekend, not on a Sunday night before my big presentation on a Monday. So we try the medication over the weekend, see how it feels (if you're not working) and then we have a sense of how you'll feel Monday morning. But give yourself a few days to figure it out.
Those are some of the things and techniques that I use to just sort of help people navigate. And again, there's something I wanted to say related to sexual side effects. There are some antidepressants that are not associated with sexual side effects so I'll just go towards those and stay away from some of the other ones that have potential sexual side effects.
Jasmine: I do wonder, like how are you deciding which ones you feel most comfortable prescribing?
Dr. Glover: I think about price. I think about this person if they're going to be using insurance and the likelihood of their insurance covering it. Just like somebody put in the chat, does it depend on the formulary? If their insurance says “We only cover this formulation of this medication. We're not going to cover the one that's long lasting because that one is still under patent, so you can only give the version that is twice a day.” Well, then I have to think, okay, this insurance only covers the formulation for twice-a-day dosing, how likely is this person going to take this medication twice a day? So I'm really trying to get to know the patient and their lifestyle.
If I know this person is homeless or unhoused, for example, do I want to send them off with a medication that's going to knock them out completely at night and perhaps leave them vulnerable to assault if they are so heavily sedated in a place where they're not safe? I really just try to customize it, is my point. If I know that somebody is in a relationship or if I know that for this person, their orgasms are incredibly important, I will bear that in mind and say we're not going to use the medications that are associated with delayed orgasm.
For example, if I know the person is struggling with weight, either their appetite is too low or their appetite is too high, then I'll think about medications that sometimes stimulate appetite or medications that turn off appetite–because those exist.
Jasmine: That was really well put. So if your psychiatrist says, “you know what, I've heard what you said, I think you are dealing with this,” and they want to prescribe you something, is it possible for you to say like, no, I don't think that's what it is. I want to be treated for this instead.
Dr. Glover: That's pretty rare. I will honestly say it's pretty rare for a patient to disagree with my diagnosis, mostly because I review the symptoms. Like okay, so you are telling me if I understand correctly, you are having difficulty falling asleep, you're feeling hopeless, having feelings of low self-worth and you have no appetite and sometimes you think about hurting yourself? That's depression, right? Five of the nine symptoms–that's depression.
Could it be more than depression? Absolutely. It could be depression and trauma. Complex trauma or PTSD. In some ways, people do come to me sometimes and say “I think I'm bipolar” and when I listen to them some more, it turns out to be a combination of emotional dysregulation, but not bipolar disorder proper. Sometimes people who grew up with a history of trauma, either childhood sexual abuse or physical assault or they grew around lots of chaos, and people who don't know how to communicate through conflict in an effective healthy way, they may have trouble regulating their emotions. That doesn't mean you're bipolar; it just means you haven't learned how to regulate your emotions and we need to work on that in therapy and with medication.
But I’ve definitely had people who said, “I don't want to take that medication. I know people who have taken that and I don't want to take it.” And then sometimes it's a matter of they will then say I want to take Adderall or I want to take Xanax, and I'm like, “Well, that has incredible street value and so that's interesting that you asked specifically for that. Can we talk about that?” Because some people are seeking medication to sell or to become intoxicated. But if somebody is willing to take something, we usually can find some sort of agreement.
Jasmine: When you were talking in the beginning about just the media in general, glorifying just, you know... I think of a movie that I was watching recently, the mom like sitting at the game and she just like starts popping stuff and she's like, oh, I’ve got to get through this. And I think like a lot of times the media, that can itself be a negative effect and make people think like, oh, that's not what I'm trying to do here. So I love that you address that and hopefully, these types of conversations will just kind of get rid of that stigma and let people know that that's not the reality of it.
Dr. Glover: Yeah, for sure. That's definitely been one of the more disheartening parts of ingesting media and some of the TV and film. It's like it gets totally misrepresented.
Jasmine: What about CBD, non-psychoactive extracts for occasional bouts of anxiety and depression?
Dr. Glover: There's not a ton of great evidence about CBD. I've heard lots of anecdotal evidence, but there haven't been really good... I mean, the gold standard in medicine is randomized placebo-controlled trials to assess a CBD tincture versus one that doesn't contain CBD but looks like it does, and giving that to people who are struggling with depression or anxiety and then measuring that for 12 weeks. That would be the gold standard. Those trials are not abundant so there's just not enough evidence.
To me, if somebody tells me, “I swear by my CBD,” I'm like, whatever, I'll work with you. If somebody tells me do not come between me and my cannabis. Or I have people on a medical cannabis program here at our hospital system. And so, for the most part, I just think like if your CBD products or if your cannabis products are enhancing your life in ways that are helping you live your best life, I'm not gonna stand in the way of that. But if there are other things that still need to be treated, I'm here for that too.
Jasmine: Perfect. I just want to close off with one more question. Someone who needs to continue with their medication or needs to take a pause or whatever that is. Like what steps do you advise people to take whenever they find themselves in a situation where they don't have the insurance to cover it? Sometimes these really, really expensive drugs.
Dr. Glover: Sometimes I'll suggest they go to GoodRX. GoodRX.com helps you locate which pharmacies carry the medication that you want and you can gauge how much it will cost you. And often you can get it for much lower prices than if you didn't check GoodRX. Like you can literally print out a coupon from GoodRx, bring it to the pharmacy, and you will pay for the medication but it'll be at a significant discount.
Jasmine: Thank you so much. This was a wealth of information. Can you let everyone know how to get in contact with you?
Dr. Glover: My Instagram is @DrKarinn. On social media, on Twitter, on Instagram, I'm Dr. Karinn. Dr. Karinn Glover on Facebook. I will also say there's a lot of black women psychiatrists and black male psychiatrists who are trying to teach our colleagues from other backgrounds how to do better and so I want y’all to pray for us. And I also want you to be aware that the medical field as a whole is undergoing massive changes, and psychiatry in particular. I think people are really trying to understand better how to not have racial trauma play out in the medical setting.
Jasmine: Glad to hear that. Well, thank you again for being here with us.
Dr. Joy: I'm so grateful Dr. Glover joined us for that conversation, and for Jasmine for doing such a great job facilitating it. To learn more about Dr. Glover and her work, be sure to visit the show notes at TherapyForBlackGirls.com/session221. And don't forget to text two of your girls right now and tell them to check out the episode as well. If you're looking for a therapist in your area, be sure to check out our therapist directory at TherapyForBlackGirls.com/directory.
And if you want to continue digging into this topic or just be in community with other sisters, come on over and join us in the Sister Circle. It's our cozy corner of the internet designed just for black women. You can join us at Community.TherapyForBlackGirls.com. Thank y'all so much for joining me again this week. I look forward to continuing this conversation with you all real soon. Take good care.