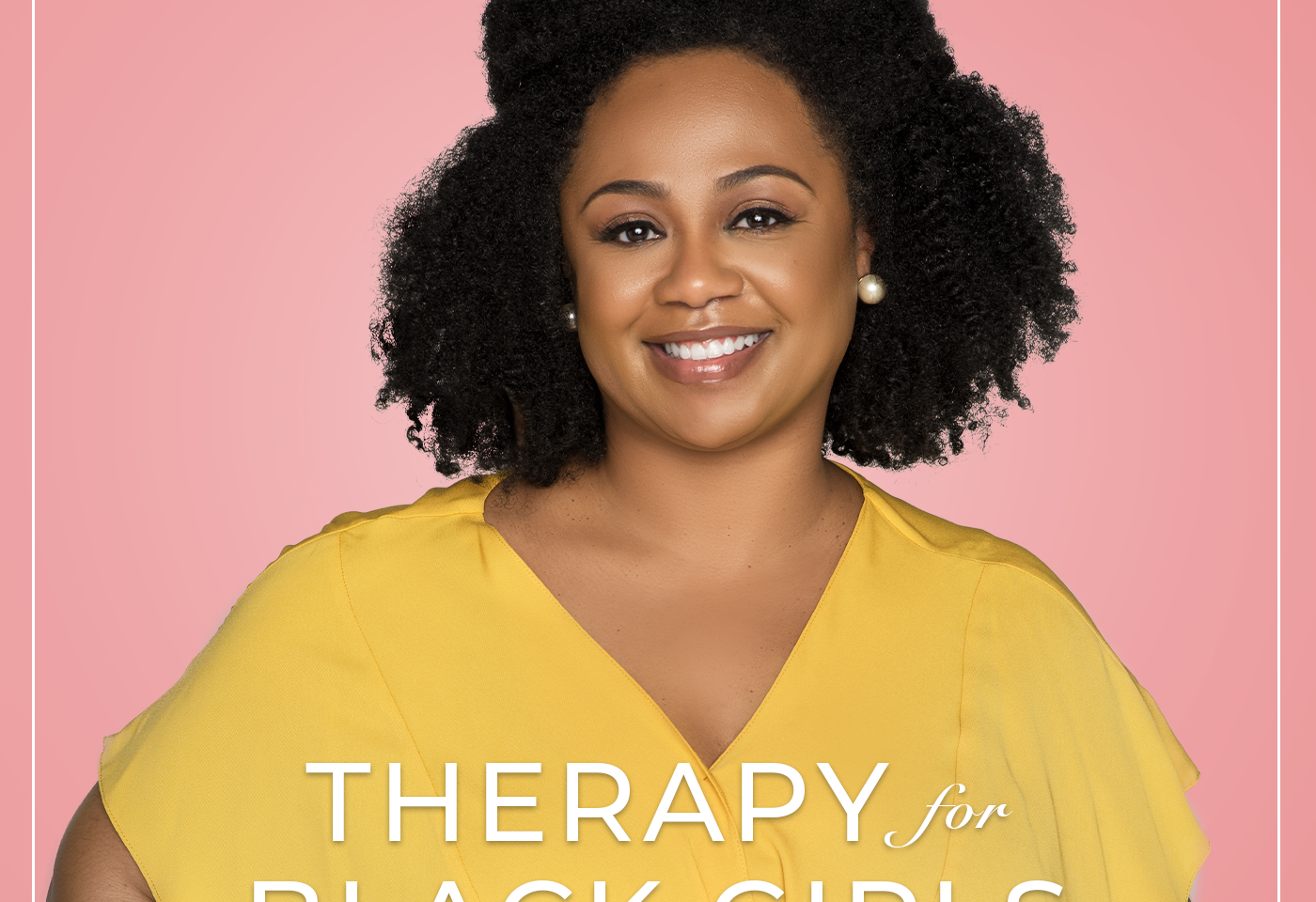
The Therapy for Black Girls Podcast is a weekly conversation with Dr. Joy Harden Bradford, a licensed Psychologist in Atlanta, Georgia, about all things mental health, personal development, and all the small decisions we can make to become the best possible versions of ourselves.
Concerns like PCOS, fibroids and endometriosis are often very painful and complicated but are also often misdiagnosed. Joining us today to chat about these gynecologic concerns that impact our health and sometimes fertility is Dr. Ashley Davis of the Fibroid and Pelvic Wellness Center. During our conversation, Dr. Davis shared about the symptoms of PCOS, endometriosis, and fibroids, what some common treatment plans might include, and things you may want to consider related to fertility.
Resources
Visit our Amazon Store for all the books mentioned on the podcast!
Where to Find Dr. Davis
https://fibroidandpelvicwellness.com/
Stay Connected
Is there a topic you’d like covered on the podcast? Submit it at therapyforblackgirls.com/mailbox.
If you’re looking for a therapist in your area, check out the directory at https://www.therapyforblackgirls.com/directory.
Take the info from the podcast to the next level by joining us in the Therapy for Black Girls Sister Circle community.therapyforblackgirls.com
Grab your copy of our guided affirmation and other TBG Merch at therapyforblackgirls.com/shop.
The hashtag for the podcast is #TBGinSession.
Make sure to follow us on social media:
Twitter: @therapy4bgirls
Instagram: @therapyforblackgirls
Facebook: @therapyforblackgirls
Our Production Team
Executive Producers: Dennison Bradford & Maya Cole
Producer: Cindy Okereke
Assistant Producer: Ellice Ellis
A Conversation on Gynecologic Health
Dr. Joy: Hey, y'all! Thanks so much for joining me for Session 232 of the Therapy for Black Girls podcast. We'll get right into the episode after a word from our sponsors.
[SPONSORS’ MESSAGES]
Dr. Joy: Concerns like PCOS, fibroids, and endometriosis are often very painful and complicated but are also often misdiagnosed. Joining us today to chat about these gynecologic concerns that impact our health and sometimes fertility, is Dr. Ashley Davis. Dr. Davis is a gynecologic specialist at the Fibroid and Pelvic Wellness Center in Peachtree Corners, Georgia. She received her Bachelor of Science at Prairie View A&M University and went on to attend medical school at the University of Tennessee. Upon graduating, Dr. Davis entered the residency program in obstetrics and gynecology at Mount Sinai Hospital in New York. She completed a postdoctoral fellow at MD Anderson's Ovarian Cancer Research Lab. She is not only board certified in obstetrics and gynecology, but has also received a Focused Practice designation in pediatric and adolescent gynecology from the American Board of Obstetrics and Gynecology.
During our conversation, Dr. Davis shared about the symptoms of PCOS, endometriosis and fibroids, what some common treatment plans might include, and things you might want to consider related to fertility. If something resonates with you while enjoying our conversation, please share it with us on social media using the hashtag #TBGinSession. Here's our conversation.
Dr. Joy: We're very excited to dig into lots of women's health kinds of topics and there have been lots of conversations and questions from our community about like fertility and things that lead to infertility, and so we really wanted to have an expert on to talk about some of these things. One of the things that has come up a lot within the community is PCOS and so I would love for you to maybe start by telling us a little bit about what PCOS is and how it can show up in our bodies.
Dr. Davis: PCOS is basically a disorder, it's a syndrome–polycystic ovarian syndrome–and it's basically a disorder of anovulation. Every month you're supposed to ovulate and that's what triggers your period but in women with PCOS, they don't ovulate and so you cannot have a period. It's also tied to a syndrome, it can be associated with prediabetes, elevated cholesterol, and sometimes obesity. The main symptom that you're going to have is one of three things–you're going to not have your cycle every month, you may have signs of excess testosterone like acne or maybe you notice some growth on your chin or your chest (excessive hair growth, you feel like you're really hairy) or having polycystic ovaries on ultrasound.
Dr. Joy: Got it. And you know, we often hear about PCOS as it's related to fertility, but my understanding is that it can predispose us to all sorts of health problems. Can you say more about how it impacts us in ways not connected to fertility?
Dr. Davis: It can predispose you to insulin resistance or predispose you to prediabetes. And really the main thing with PCOS that I try to explain to my patients is when you are not on any hormonal therapy and not having a cycle, it's very unhealthy for your uterus. Because every month, when your body doesn't get that signal to have a cycle, the lining can continue to build up and that can put you at higher risk of cancer or pre-cancer of the lining of the uterus. When we're treating PCOS, that's really the main thing we're trying to prevent, is making sure you have a cycle so you're not predisposed to that.
Dr. Joy: And so when you have patients that come to you who think they may have PCOS, is having a missed cycle typically the first symptom they have, or how might we know this might be something we're struggling with?
Dr. Davis: If you don't have a cycle every month. If you're not having a cycle at least Every 21 to 35 days, you definitely need to be evaluated for PCOS. There's other things that can cause missed periods as well like thyroid disease, prolactin, but PCOS is very common and so you definitely need to be worked out for that.
Dr. Joy: Got it. What are some treatment options for somebody who has been diagnosed with PCOS?
Dr. Davis: First, I said like the main thing is we want to get your period back to protect the lining of your uterus so you're not predisposed to cancer of the lining of the uterus. That looks like some form of usually hormonal therapy, like birth control pills or a Mirena IUD–it's an IUD that has some progesterone in it that keeps the lining of the uterus thin. It also involves lifestyle changes. Because you are at higher risk of developing high cholesterol and insulin resistance or prediabetes, I like to send my patients to a PCOS nutritionist that can help them with the lifestyle changes. Sometimes that includes weight loss, sometimes it doesn't, because not all PCOS patients are overweight so they can optimize their diet for that lifestyle.
And then hormones are not the only medications available. Sometimes we can use things like Metformin which is a diabetes medication, and then sometimes that therapy is just targeted at some of the other symptoms of the high testosterone like the acne and excessive hair growth, and you can use other medications like Spironolactone for that.
Dr. Joy: Dr. Davis, might you be on maybe a couple of those medications, depending on what your symptoms are?
Dr. Davis: Exactly, exactly.
Dr. Joy: Ah, okay. And I would imagine that may be difficult, especially for people who maybe don't like to take a lot of medicine
Dr. Davis: Yeah, of course.
Dr. Joy: Can you talk a little bit about like maybe how you talk to patients about this and what their treatment plan looks like?
Dr. Davis: I find that a lot of people, they've been told they have PCOS and they’re given a birth control pill and they're not told why they need it. And they're like, I don't want to take this, it makes me feel crazy or you're worried about weight gain. And when I really explain to them why we're giving you hormone therapy, we're really trying to protect the lining of your uterus, keep your uterus healthy so you can conceive one day, they're usually more accepting. There's a lot of different forms of birth control and hormonal therapy, some that you don't even have to take every day of the month. So just finding a doctor that's open to having that conversation– that’s not just giving you a pack of pills and saying, “hey, take this,” but giving you all the alternatives.
Dr. Joy: Got it. And so is this something that maybe you're on this medication for like six months to a year and then we see it subside, or is this something that they typically have to be on for like the rest of their lives?
Dr. Davis: It depends. I've definitely had patients that noticed that some lifestyle changes–either if they are overweight, sometimes losing weight, or even if they're not overweight, doing the lifestyle changes like I talked about, speaking to nutritionists, exercising–they're able to get their period back. And you can have PCOS and reach a stage where you are having a regular cycle, in that case you don't need to be on hormonal therapy.
Dr. Joy: Got it, okay. So really, we are trying to do whatever we need to do to make sure that we do have the regular cycle?
Dr. Davis: Exactly.
Dr. Joy: Got it. Because that's your main concern, is that we don't want the uterine lining to thicken so that it predisposes you to a cancer.
Dr. Davis: You’ve got it spot on.
Dr. Joy: Listen to me talking like I have gone to somebody’s medical school!
Dr. Davis: That’s excellent!
Dr. Joy: Thank you, I appreciate you breaking that down. Because you know, sometimes like there's all these big words and it can be sometimes difficult to understand, so I appreciate you sharing in a way that makes it really understandable for people, like why this is a concern.
Dr. Davis: Yes, I think that's super important and you need to speak the patient's language. You have to be able to communicate with your doctor.
Dr. Joy: Yeah, thank you for that. Something else that when we told people we were having an expert to come on and talk about some of these women's health concerns, it seems like there's a little bit of a misconception, or you can tell me whether this is a myth or a fact. Are black women more prone to PCOS compared to other ethnicities?
Dr. Davis: I think that is a myth. Hold on, I'm gonna fact check it.
Dr. Joy: We love a fact check!
Dr. Davis: No. I think that is a myth. I mean, it's a very, very common condition and it can affect a lot of women.
Dr. Joy: Mm hmm. But there's nothing that that you've read or studied that would indicate that black women have a higher risk for PCOS?
Dr. Davis: No.
Dr. Joy: Got it, okay. Something else that comes up as a part of this conversation is endometriosis and I know that there are some similarities between endometriosis and PCOS. Can you talk about the differences? And is it possible for somebody to have both?
Dr. Davis: It's definitely possible for someone to have both. Endometriosis, the definition of that is when you have the tissue that's supposed to be inside the lining of the uterus is actually outside the uterus. It can be in the pelvis, it can be anywhere in the body, most commonly found in the pelvis, and those implants of endometriotic or endometrial-like tissue cause inflammation that can cause pain and a host of other problems. It can cause infertility, pain with sex, bloating, gastrointestinal symptoms, and it can also cause irregular bleeding.
And I definitely have patients who have endometriosis and PCOS and it can really cloud the picture because they're not getting a period every month, but when they do get their period, it's really, really painful. They have some of the other like elevated cholesterol, prediabetes (that are associated with the PCOS) on top of dealing with the pain. The main symptom of endometriosis, 80% of patients are going to present with pain and that's going to be their main symptom, whereas with PCOS, their main symptom is going to be “I'm not having my period every month.”
Dr. Joy: And so, is the pain with endometriosis typically when you get your cycle or is it like pelvic pain all the time?
Dr. Davis: It typically presents as being worse with your cycle. Having a cycle that is so painful that you're not able to go about your daily activities. Like if they're saying, Doc, I have to miss work when I have my period or I have this history of I had to stay home from school every month, I throw up, I pass out. That is not normal and that really clues us in that this may be endometriosis. The longer that it goes untreated and undiagnosed, it can progress to you having pain with sex, it can progress to you having pain all the time or pain the week before your period and not just on your period, so it can present in a lot of different ways.
Dr. Joy: When you said like pain before your period, it made me think of PMDD. Some women talk about having PMDD experiences–can you talk about like what's the difference between that and endometriosis?
Dr. Davis: PMDD is really a mood disorder. Does that make sense? Whereas endometriosis is a pathology like in the pelvis. It is associated with the hormonal changes that happen leading up to your cycle whereas PMDD kind of describes the symptoms that affect the mood–when we can have severe depression, anxiety, become suicidal because of that. However, if you have endometriosis and you’re in severe pain and you're vomiting and you can't go to work, of course, you're going to be more likely to be depressed so those symptoms can commingle and people may think they have PMDD but really it’s you're just in a lot of chronic pain and that can definitely affect your mood.
Dr. Joy: Mm hmm. More from my conversation with Dr. Davis after the break.
[BREAK]
Dr. Joy: As you're talking, Dr. Davis, it definitely sounds like so much of this can sound like the other thing. And so I'd love for you to be able to share at least a little bit, or whatever you can, around like how you make decisions depending on what your clients come in to you saying they're concerned about.
Dr. Davis: The main difference is going to be pelvic pain with PMDD versus when patients maybe come with a presenting symptom of they have anxiety or depression around their period. And I'll ask them, how are your periods? How long are your periods? If they're lasting 10 days, of course that's going to affect you. Do you have pain with your periods? And anybody that has pain with their cycles, I'm going to be very suspicious. Severe pain with their cycles that keeps them from doing their day to day activities, that's not relieved by ibuprofen or Midol, I'm going to be concerned about endometriosis.
Dr. Joy: Got it. Okay, and what might a treatment plan for endometriosis look like?
Dr. Davis: Initially, it can start with hormonal therapy. Especially for women who their pain is just with their cycles, giving them medication or hormonal therapy, or like the IUD where you don't have a cycle at all, it can definitely help with those symptoms. When they don't have a period, they don't have the pain and it can really change their life. What's important and where a lot of physicians go wrong is we're kind of taught that birth control pills are the first line of therapy for endometriosis, but they don't work for everyone.
And so it's really important that you have a good relationship with your physician and are able to advocate for yourself and say, hey, I tried this treatment but it's not working. I'm still in pain, I'm still not able to function. I still have pain in between my cycles and we need more evaluation. No one should be diagnosed without at least getting a pelvic ultrasound. You can't see endometriosis on a pelvic ultrasound, but it can rule out other things.
Dr. Joy: Okay, so you're trying to not necessarily see endometriosis but you're trying to rule out whether there's something else is going on.
Dr. Davis: Exactly.
Dr. Joy: Got it, okay. You mentioned that a lot of people are trained to use birth control as the first line for a lot of things. And when you talked about the pain that comes with endometriosis, and we know how often black women talk about like how doctors don't believe their pain, I'm wondering if you can talk a little bit about maybe some of the medical biases that might make it difficult when black women go in for treatment for some of these concerns.
Dr. Davis: Well, of course, there's a history of racism in medicine. Medicine was established in slavery, a lot of our gynecologic procedures were developed and discovered by practicing on enslaved women without their consent, so there's a history there. And actually, being an OB-GYN, that used to be a very male dominated field because it's a surgical field and so there's a long history of them kind of being paternalistic and thinking they know what's best for a woman rather than a woman giving her complaints and us working together and trying to find a treatment plan.
And so people will find that when they come with their complaints, as soon as they open their mouth, their doctor already has an idea of what's wrong with them–oh, this could just be fixed with birth control pills. And so when you go to the doctor, one thing that you need to look for is somebody that takes your concerns seriously and that offers you some type of diagnostic testing. And you are also allowed to request that if that's not what's offered.
Dr. Joy: Can you say more about like asking for some of these tests that are not offered?
Dr. Davis: Anybody with any type of period complaint, if you're in pain, if your period is too long, you need a pelvic ultrasound and I think that that step is often missed. That's kind of looked over, we'll say we'll try medication first and see if it gets better, whereas I think we should always start with the pelvic ultrasound so we can actually make an effort to diagnose what's going on. And if the doctor says, oh, you know, let’s start you on the medication first and see how you do, you ask, “Hey, I would actually think I should get a pelvic ultrasound. What do you think about that? Do you think that'd be a good idea?” And most of the time, physicians do care, they will acquiesce and if your patient is asking for a test and it is indicated, they will give it to you. If not, there's other doctors.
Dr. Joy: Right. I think you bring up a good point, like if you are going to a doctor and you ask for a test that you think could help to rule out some things or give more information and the doctor isn't willing to do that, that may be a sign that you might need a new provider.
Dr. Davis: Exactly. Or explain. If they're not able to articulate to you why you don't need it and it doesn't make sense to you, you can always get a second opinion. That's never going to be harmful at all. So yeah, I would encourage people, yes, get a second opinion because you need to be sure about your treatment plan. You need to know what's going on with your body.
Dr. Joy: Are there any like specific diets or lifestyle changes that somebody can make that helps to curb the symptoms of either PCOS or endometriosis? You talked about maybe something related to nutrition to try to get diet under control, but are there other things you’d suggest?
Dr. Davis: There's no like discreet evidence that this lifestyle intervention affects your pain or can affect endometriosis pain. For PCOS, it’s different because sometimes weight loss, avoiding carbs, obviously avoiding cholesterol and fat if you have elevated cholesterol, will affect PCOS. But with endometriosis, I typically tell people to try to just have an anti-inflammation diet, have a healthy diet, lots of fruit and vegetables. Avoiding what's called exogenous estrogen, so any foods with a lot of estrogen, there's things that we put in our lotions that we use, and just trying to basically use... I don't like to say clean ingredients, but trying to avoid extra hormones. And even sometimes it’s in birth control pills, I see that for my fibroid and endometriosis patients.
And I think you have to figure out what works for you. I wish there was a diet I could prescribe that I knew would help everybody. I think it's about researching about lifestyle changes and seeing if you notice that if you're exercising more that your periods are not as bad or your pain isn't as bad. If you're avoiding certain things–some people cut out meat and that helps them, some people cut out dairy and that helps them–to see how it goes.
Dr. Joy: So it really is just trial and error?
Dr. Davis: Yes, exactly.
Dr. Joy: For a lot of it, got it. Something else, Dr. Davis, that has come up a lot. Most recently Tiffany Cross had a segment on her Saturday morning show, The Cross Connection, where she talked about like having surgery for her fibroids. And so many people, it seems like, have these stories about these orange size, lime size, like different size fibroids that they end up having to have surgery for. Can you talk a little bit about what fibroids are and like how they develop?
Dr. Davis: Fibroids are benign or non-cancerous tumors or growths of the muscle tissue of the uterus. They typically develop in the muscle lining of the uterus or they can be anywhere on the uterus. We don't know exactly what causes them or why they start, but they can grow and they usually cause heavy bleeding. They can also cause pain, pelvic pressure, and in some cases, about 10% of the cases, infertility.
Dr. Joy: Do they always require surgery or do they like go away by themselves sometimes?
Dr. Davis: They don't go away by themselves, they're always gonna be there. Everyone's different so some women may have a one-centimeter or a grape-sized fibroid and it stays that way for years. Other people have that sized fibroid and it grows to the size of a lime in two or three years and there's people that it will grow to the size of a cantaloupe in one year. So it's different in everybody. We know that those tumors are sensitive to estrogen and estrogen is what your body makes every day, that's what makes you a woman, that’s what your ovaries make. And so they're very common that they will grow.
The majority of fibroids are not symptomatic, like women don't have symptoms of heavy bleeding, they may find them incidentally on an ultrasound or some other form of imaging. And in those cases, you don't need to do anything if you don't have any symptoms of heavy bleeding or pain. But we should always keep an eye on them to make sure they're not growing rapidly, so that means an ultrasound at least every couple of years or every year, or your doctor examining you to make sure they're not progressing.
If they are symptomatic, we could again use medications, some hormonal therapy, some non- hormonal therapies that can slow down the bleeding that can be associated with the fibroids. And then there's surgical options, and not all those options are hysterectomy, that's super important to say.
Dr. Joy: And is that one of those things too where a lot of physicians will kind of rush to a hysterectomy as opposed to trying some other thing?
Dr. Davis: Yes, and historically especially for black woman. Because there's a history of forced sterilization of black women in this country, where they're sterilized against their will, and when a hysterectomy is one of the ways of doing that. Yes, some doctors if they offer you the first thing–especially if you're young and you haven't had children–and they say the first thing you need is the hysterectomy and they don't talk to you about every single option, you need to get another opinion.
Dr. Joy: Yeah, it definitely seems like it would be that kind of thing, especially maybe physicians who have been trained for a long time...
Dr. Davis: Yes, exactly.
Dr. Joy: Where that may be their first line of defense.
Dr. Davis: Yeah, it should not be the first thing that's talked about at all.
Dr. Joy: Right, got it. And so how can fibroids impact your fertility?
Dr. Davis: Fibroids impact fertility if they're in the lining of the uterus. The baby needs to implant on the inside of the uterus in the uterine cavity, and if a fibroid is either pressing in on that cavity or actually inside the cavity, it can interfere with implantation. Or if it's blocking the fallopian tube–that's the tube where the egg needs to get from the ovary into the uterus. But it's rare that they're in that location, so again, that's about 10% of the time that it's affecting fertility.
Dr. Joy: Got it, okay. Tiffany mentioned, when she was talking about it, like one of her symptoms was that her hair was falling out and she knew because it had also happened to her mom. And I had not heard of like hair loss as being related to fibroids. Can you talk about that?
Dr. Davis: Well, that's because of the anemia. The anemia of the women, and I've seen this come in their first complaint, maybe that their hair is falling out or they feel tired, and they find that they're anemic. And you'd be surprised how many times physicians don't look closely at, okay, what is causing this anemia? And women may not tie it to their period because their periods have always been seven to 10 days and really heavy, and they think that's normal for them. They don't recognize that they're losing so much blood, it's making them sick.
Dr. Joy: Yeah, because I could imagine if hair loss was your first symptom, you probably would start with like your primary care doctor or maybe a dermatologist. And if they found that you were anemic, they would put you on some kind of iron supplement, I'm guessing. And so how would you then connect that to maybe a fibroid or something? Like who would ever know to think about that?
Dr. Davis: They should know. They should know, that's the point.
Dr. Joy: So my non-physician training would not let me know, but a physician who is doing it...
Dr. Davis: A physician should know.
Dr. Joy: Got it.
Dr. Davis: If you have a patient with anemia, we need to we need to figure out, okay, why are you anemic?
Dr. Joy: Got it, okay.
Dr. Davis: Yeah, and there's some bloodwork we can do to see if it's iron deficiency anemia, which is usually associated with blood loss. We have seen patients who have been going to a hematologist and getting IV iron and no one's talked about, okay, why are they bleeding?
Dr. Joy: Okay, so it is sometimes missed?
Dr. Davis: Yes, it is. Unfortunately. So it's important to have these types of podcasts where patients know what to look for, how to look for the signs and symptoms, and I can tell you that if you are bleeding so heavily that you're bleeding through your clothes, that you feel weak and tired on your cycle or your period lasts more than seven days, that needs to be evaluated.
Dr. Joy: More from my conversation with Dr. Davis after the break.
[BREAK]
Dr. Joy: Are there other things that you've seen like that, Dr. Davies, that you feel like, oh, I really wish more people knew about this?
Dr. Davis: I would love for them to know that there's an average of three to five years before women get treated for their fibroids and it's usually because they're scared. They're scared of surgery, they're scared of the treatment options, they're scared of gaining weight on birth control pills or because they've never tried them. And I would just say that I really want them to try to find a doctor that they can trust that will go over all the options with them, so they can feel comfortable making their decision and not to just suffer. So many women, they suffer for so long before they get help.
And it's a personal story. Like my mom had fibroids and endometriosis and suffered for years that I saw growing up, she would be in pain during her cycle, she would kind of disappear. And it wasn't until like I was an OB-GYN and started learning about them in medical school and I was like, “Ma, I don’t think what you're going through is normal. I think you may have endometriosis.” She's like, well, no one's ever told me that. And she ended up having a hysterectomy later when she was in her 50s. And she suffered for so many years.
Dr. Joy: You bring up a really good point. We had a conversation in an earlier session with Dr. Sara Flowers, I think her name is, just about like socialization related to our cycles. And so hearing you talk about your mom being in so much pain, I think a lot of our moms and grandmothers just talked about like being in pain. And we then grow up thinking like, okay, we're just supposed to like suffer this pain for a couple of days out of a month, but it actually could be something else going on.
Dr. Davis: It can be serious and it can be something that's treatable and it doesn't mean that you have to have a hysterectomy. And hysterectomy is the right choice for some people and other circumstances, but you deserve to just go through all the options. It's so funny, some of my patients, they come in knowing that they want a hysterectomy because they've completed having their children and I still go through all of the options, all the medications. They're like, can we just skip to the last one? I'm like, no, we’ve got to go through everything.
Dr. Joy: Just want to make sure we explore all the options! You've already talked a lot about using hormonal things to kind of address some of these other concerns, but I'm wondering for people who maybe are thinking like, okay, I want to start maybe some kind of birth control. Can you talk to us about the different kinds of birth control that exist, and then how you make decisions about maybe what is the best one for your patients?
Dr. Davis: I let the patients decide what's the best one for them but there are so many different types. The one that people know about the most is pills and that's something you have to take every day. It's a combination of estrogen and progesterone together that works similarly to your cycle and you can have a cycle every month. It's cycle-simile to your normal hormones, that's one of the easiest things. But estrogen-progesterone combination comes in a pill form, a patch form and a ring form. The patch, you have to change once a week, the ring, you have to change once a month. And so it really kind of just depends on how much daily effort the patient wants to put in.
Another favored option is the IUD, intrauterine device. There's two kinds, one that has hormones and the hormones are very localized. I think it's a great option for people that want to minimize their exposure to hormones because most of the action is local, because it's inside the uterus. It keeps the lining of the uterus thin and prevents pregnancy that way, and it can last for five years. And you have a small amount of progesterone only, there's no estrogen in it that's in your bloodstream, so the side effects are very minimal.
And there is an IUD that has no hormones that lasts for 10 years, but it makes your periods heavier and longer and more painful. And most of my patients are already suffering with that so it's not something that I use that often, but it's still there and a good option. There's other long- acting ones like the implant, the contraceptive implant called Nexplanon, it lasts for three years. It's another progesterone only form. The main side effect with that one is it can sometimes have irregular bleeding, but there's patients who do great with it. I think that the most important thing that people need to recognize, like when they're looking at birth control options, everyone's freaked out by potential side effects. Try it and see what it does and if you want to discontinue it or you want to try something else, we try something else.
Dr. Joy: Got it, thank you for that. Yeah, it does seem like there are so many different choices. Back when like I was in college like thinking about birth control, all of these options did not exist so it's good that there are so many different options and you can pick. Like you said, okay, let me try something and see how it works and maybe that is a good one or maybe I try something else.
Dr. Davis: Exactly, you're not locked in. And the pill is not associated with weight gain in the studies. I know that it happens to some people so you just have to see how it works for you.
Dr. Joy: Mm hmm, yeah. What are some of the questions that young women should be asking themselves regarding fertility? We often hear about this biological clock and you only have so many years. First of all, is the biological clock real, like are we working against the clock?
Dr. Davis: It is, unfortunately. It is not fair but it’s real.
Dr. Joy: Got it, okay. Some people may know that they want children later, maybe people are undecided. What kinds of things should people be thinking about in their youngest years–maybe, you know, 18 over–about their fertility and like how to maybe have some of those options open for later?
Dr. Davis: The most important thing they can do is wrap it up. Chlamydia is the number one cause of infertility because it can scar your tubes. So just thinking about overall protecting your space, protecting your organs, making sure that you're having safe sex with a partner that's tested, I think that is the number one thing. The second is keep an eye on your periods. If your periods are painful or they last longer than seven days, to seek evaluation to make sure that your uterus stays healthy. You have PCOS, you're making sure that your uterus stays healthy, that you're taking the medications or the precautions or lifestyle changes, whatever you and your doctor decided to make sure you're having your cycle. And unfortunately, we have to think about age. Your fertility does decline as you get older. The perfect solution is to freeze your eggs when you're in your early 30s or late 20s.
Dr. Joy: Are those conversations that you are frequently having with patients, about freezing eggs?
Dr. Davis: It is. It's not talked about enough and (unfortunately) it's not accessible to everyone because it can be so expensive, but it's like an insurance policy. You know, if you don't meet Mr. Right until you're in your late 30s or early 40s, if you have your eggs frozen, then you don't have to worry about settling. The other thing, especially my patients with endometriosis because endometriosis can affect fertility, I've had several young patients that are diagnosed when they're 22, 23–go ahead and freeze their eggs so they keep their options open later.
Dr. Joy: Got it. Are there other things that impact fertility that we haven't talked about?
Dr. Davis: A lot of infertility is unexplained. About 30% of women that are unable to conceive, we don't actually find a reason. But it can be your ovarian reserve (how many eggs you have left) which are affected by your age and sometimes they’re low and it could be affected by endometriosis. You have to make sure your tubes are working, the connections between your uterus and your ovary. That can be affected by infection, by previous surgery, by fibroid sometimes. And then your uterus being healthy, so making sure your endometrium is normal. If you have PCOS, making sure there's no fibroids in the way. And then male factor–the man has responsibility in this too. In 30 to 40% of the time, it's because of the man.
Dr. Joy: Got it, okay. You know, when we're thinking about like our fertility options, are there any tests we can ask for from a doctor about like testing fertility and those kinds of things?
Dr. Davis: It depends on where you are. The diagnosis of infertility is when you're not able to get pregnant for a year. When you haven't been trying to get pregnant, it's harder to predict, like am I going to be able to get pregnant? If you're having normal cycles, it’s likely that you're ovulating every month, and you're not having pain with your cycles, your cycles aren’t long, it's reasonable to assume that everything is healthy.
Another test everyone asks about is the AMH or Anti-Müllerian hormone, and that gives us an idea of your ovarian reserve. That test was actually developed to see how well people would respond to infertility medications. We kind of use it to determine how many eggs a woman has left, but it really wasn't developed for that. And it doesn't affect your ability, even if your AMH is low, to be able to get pregnant naturally. So that test, I know there's a lot of over the counter testing available for the AMH, but just make sure that you have a conversation with your doctor about those results so you don't freak out and think that you're infertile just because you have a lower number.
Dr. Joy: Okay, so is that testing like you can do on your own?
Dr. Davis: Yeah, I know there's a lot of companies that they have you doing it on your own. But I suggest going in and having a conversation with your doctor about those tests so you know how to interpret it, and we can ask you those questions about your uterus, about your periods about your symptoms. And I always ask about everybody's timeline. Are you dating anyone or like what's your plan? Because some people are like I know I want to get pregnant in the next year, some people are like I don't know if I even want to get pregnant or it’s just not in them, you know, and all of that is important in this discussion.
Dr. Joy: Is there a certain age at which you start having this conversation and maybe about egg freezing with your patients?
Dr. Davis: I have it early because the younger you are, the better. Especially my patients if they have endometriosis. So I offer it to everyone, I talk to everyone about it and let them make the decision. It's such a personal decision, you know, it really is.
Dr. Joy: And it's not something that you do with them in office. They would need to go to another kind of a physician?
Dr. Davis: Yes, they would need to go to an infertility physician and I have a lot of fertility physicians I can refer them to.
Dr. Joy: Perfect, perfect. Are there any resources that you find yourself suggesting to patients often, related to some of the topics that we've talked about?
Dr. Davis: I think it's important to have a support group. There's a lot of great endometriosis support groups that they can find, and fibroid support groups, so they just know that they're not alone. And women are great at sharing resources so you can just get information. I tell everyone they should do their internet research on the things that I'm suggesting so you can come up with questions and you can come back and ask or message me questions. Do your own research but kind of with the guidance of a doctor that you trust.
Dr. Joy: Yeah, I think that that's important because we are especially hearing a lot about people doing their own research right now, but we also want to check in on that research with somebody with the appropriate credentials.
Dr. Davis: Because if you google everything, you know, they'll tell you that you're about to die.
Dr. Joy: Right, don't scare yourself on WebMD and stuff. Dr. Davis, tell us where we can find you. Please share your website as well as any social media handles you'd like to share.
Dr. Davis: You can find me on Instagram @AshleyDavis_MD. I practice in Atlanta Georgia at the Fibroid Pelvic and Wellness Center with Dr. Soyini Hawkins, I'm sure many of you have heard of her. Our website is FibroidAndPelvicWellnessCenter.com.
Dr. Joy: Perfect. Thank you so much, Dr. Davis. I really appreciate you sharing with us today.
Dr. Davis: Thank you.
Dr. Joy: I'm so glad Dr. Davis was able to share her expertise with us today. To learn more about her work, visit the show notes at TherapyForBlackGirls.com/session232. And don't forget to text two of your girls and tell them to check out this episode as well.
If you're looking for a therapist in your area, be sure to check out our therapist directory at TherapyForBlackGirls.com/directory.
And if you want to continue digging into this topic or just be in community with other sisters, come on over and join us in the Sister Circle. It's our cozy corner of the internet designed just for black women. You can join us at Community.TherapyForBlackGirls.com. Thank y’all so much for joining me again this week. I look forward to continuing this conversation with you all real soon. Take good care.